Key Takeaways:
- Since glioblastoma is one of the most aggressive types of brain cancer, novel therapeutic strategies are needed.
- Recent research has focused on immunotherapy, targeted therapies, and precision medicine.
- Collaboration between researchers and healthcare providers is crucial to improving patient outcomes.
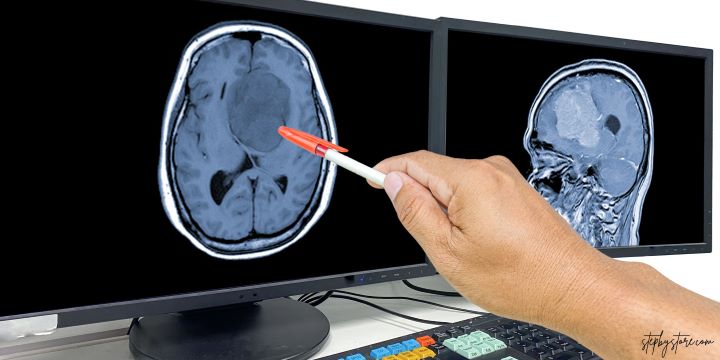
Introduction to Glioblastoma
Glioblastoma is a formidable and intricate kind of brain cancer that presents noteworthy obstacles for both patients and medical professionals. The prognosis for glioblastoma is still bleak despite advancements in medical research, underscoring the critical need for fresh approaches to therapy. With initiatives like glioblastoma awareness day, there is a growing emphasis on raising awareness and funding for research to combat this devastating disease. Awareness days are crucial in spotlighting lesser-known medical conditions and rallying public support for research efforts.
In recent years, significant strides have been made in understanding the underlying biology of glioblastoma, leading to the development of novel treatment approaches. This essay will examine the most current advancements in glioblastoma research and innovative treatment strategies that provide new hope to patients worldwide. From immunotherapy to precision medicine, scientists work tirelessly to uncover practical solutions for this formidable disease.
Immunotherapy: Harnessing the Body’s Defense System
Immunotherapy has emerged as one of the most promising avenues in the fight against glioblastoma. This innovative approach leverages the body’s natural defense mechanisms to target and destroy cancer cells. Unlike traditional therapies, which often have widespread effects on the body, immunotherapy aims to specifically activate the immune system to recognize and attack glioblastoma cells.
Various immunotherapeutic approaches are currently being explored in glioblastoma treatment. For instance, immune checkpoint inhibitors obstruct the immune system’s proteins to defend against cancer cells. This improves the immune system’s ability to identify and eradicate tumor cells. CAR T-cell therapy, another form of immunotherapy, involves modifying a patient’s T-cells to target cancer cells better. These modified T-cells are returned to the patient to seek out and destroy glioblastoma cells.
Clinical trials for these immunotherapeutic approaches have shown promising results, with some patients experiencing significant improvements in survival rates. However, challenges remain, and researchers continually work to optimize these treatments and expand their applicability. Future immunotherapies for glioblastoma will require comprehending the complex interactions between the illness and the immune system.
Targeted Therapies: Precision in Action
Targeted therapies represent another crucial advance in glioblastoma treatment. These therapies focus on specific molecular targets involved in cancer growth and progression. Treatments can inhibit tumor growth by pinpointing these targets while minimizing damage to healthy tissue. This precision approach contrasts with conventional therapies, often affecting cancerous and healthy cells.
A notable study on targeted therapies has shown promising results. Researchers have identified various molecular pathways that are dysregulated in glioblastoma, providing new targets for treatment. For example, inhibitors targeting the PI3K/AKT/mTOR pathway, often overactive in glioblastoma, have shown potential in preclinical and clinical studies. These drugs slow tumor growth and promote cancer cell death by inhibiting this pathway.
Another example of targeted therapy is drugs that block the activity of specific growth factor receptors, including the epidermal growth factor (EGFR) receptor. Mutations in the EGFR gene are commonly found in glioblastoma, and targeted therapies that inhibit EGFR signaling have demonstrated some success in clinical trials. While challenges such as resistance to targeted therapies remain, ongoing research continues to refine these treatments and identify new targets for intervention.
Precision Medicine: Personalizing Treatment
Precision medicine takes a tailored approach to cancer treatment, considering the unique genetic makeup of each patient’s tumor. This personalized approach can improve treatment efficacy and reduce the likelihood of adverse effects. Healthcare providers can identify specific mutations driving glioblastoma growth through genomic sequencing and design targeted treatment plans accordingly.
One essential advancement in precision medicine is comprehensive genomic profiling to identify actionable mutations in glioblastoma tumors. By analyzing the genetic alterations in the cancer, oncologists can choose treatments based on which ones are most likely to work for each patient. Recent advancements in precision medicine have shown that this strategy may help glioblastoma patients live longer and with better results.
For example, a patient with a specific mutation in the IDH1 gene could profit from a focused treatment that stops the mutant enzyme from functioning. Similarly, patients with alterations in the MGMT gene involved in DNA repair may respond better to certain chemotherapies. By eliminating medicines that are less likely to be helpful, this degree of customization maximizes the effectiveness of therapy and reduces needless side effects.
The Role of Collaborative Research
Progress in glioblastoma treatment is heavily reliant on collaborative research efforts. By pooling resources, knowledge, and expertise, researchers can expedite the creation of innovative medicines and enhance patient outcomes. Collaborative initiatives, such as multi-institutional clinical trials and international research consortia, are essential for advancing our understanding of glioblastoma and uncovering new treatment avenues.
Multi-institutional clinical trials allow researchers to enroll more patients, thereby increasing the statistical power of the studies and enabling the evaluation of new treatments more quickly. International collaborations bring together diverse research perspectives and access to unique patient populations, further enriching the research landscape. These collaborative efforts have already led to significant breakthroughs and continue to drive innovation in glioblastoma research.
The Glioma Connectome Project is one such project that seeks to map the molecular and cellular relationships of glioblastoma comprehensively. The project also aims to identify novel therapeutic targets by integrating data from various research groups and develop more effective treatment strategies. Collaborative research also extends to sharing data and resources, such as biobanks and patient registries, which are invaluable for advancing our understanding of this complex disease.
Improving Patient Quality of Life
The quality of life for glioblastoma patients is crucial, and supportive care measures, such as palliative care and symptom management, are essential for coping with the physical and emotional challenges of the disease. Comprehensive glioblastoma care involves holistic approaches that address the needs of patients and their families. Palliative care relieves symptoms and improves overall well-being, including managing headaches, seizures, cognitive impairments, and other neurological symptoms. In addition to medical interventions, supportive care includes psychological and social support, such as counseling services, support groups, and educational resources. Rehabilitation services like physical and occupational therapy can enhance functional abilities and quality of life. Supportive care measures contribute to a more comprehensive and compassionate approach to glioblastoma treatment by focusing on patients’ holistic well-being.